Written by Megan Winzer
As a high school student who had a keen interest in science and a passion for healthcare, nuclear medicine was the right choice for me and it could be for you too!
I really enjoy the scientific and technical aspects of nuclear medicine, however, the main thing that drew me to a career was the patient care component.
Technologists can spend up to several hours with patients and we are able to form connections with them and become quite involved in their care.
The career is incredibly rewarding, as well as working with like-minded individuals.
Nuclear medicine is a branch of medical imaging that specialises in the imaging of the function of specific cells and organs within the body.
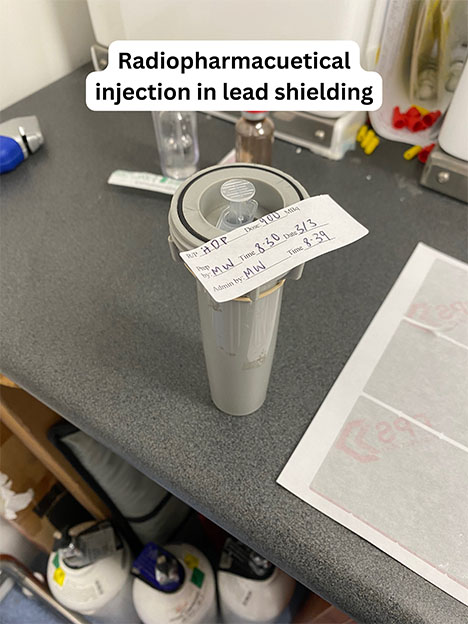
It involves administering a patient with a radiopharmaceutical which is comprised of a small measured amount of radiation chemically bound to a substance (pharmaceutical) that is naturally utilised within the body.
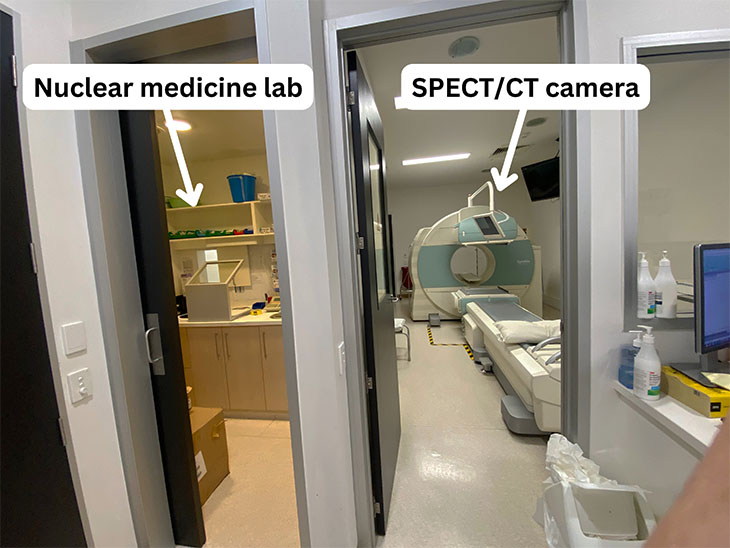
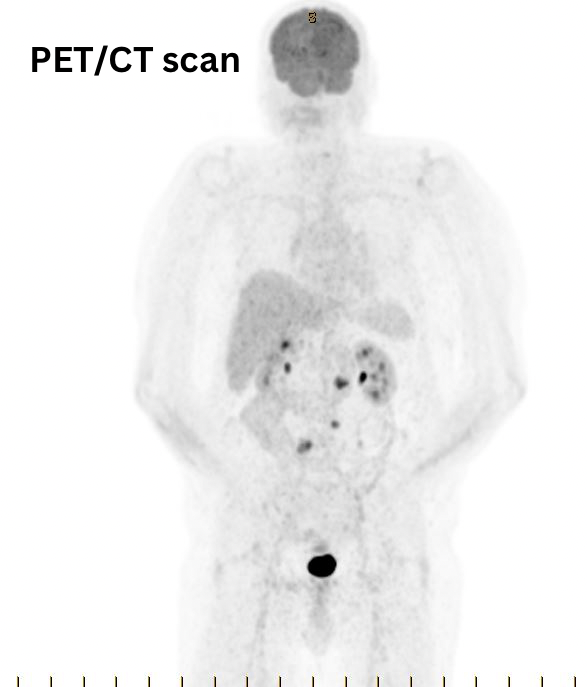
We use cameras that image the radioactive emissions from within the patient called a SPECT (single photon emission computed tomography) or a PET (positron emission tomography) camera.
We can also use hybrid imaging where a low radiation dose CT is overlayed with our emission images to allow radiologists to view the patient’s anatomy as well as the function.
Something really amazing about nuclear medicine is not only can we perform imaging but we can also provide treatment for diseases such as cancer and thyroid disease using highly specialised radiopharmaceuticals with a much higher radiation dosage to target and kill any diseased cells.
Here’s a look at a day in nuclear medicine with one SPECT/CT camera:
7am
Perform the radiation elution from the generator.
Make the radiopharmaceuticals for the day (each different type of scan generally requires a different radiopharmaceutical to be made everyday).
Perform quality control on the camera.
8am
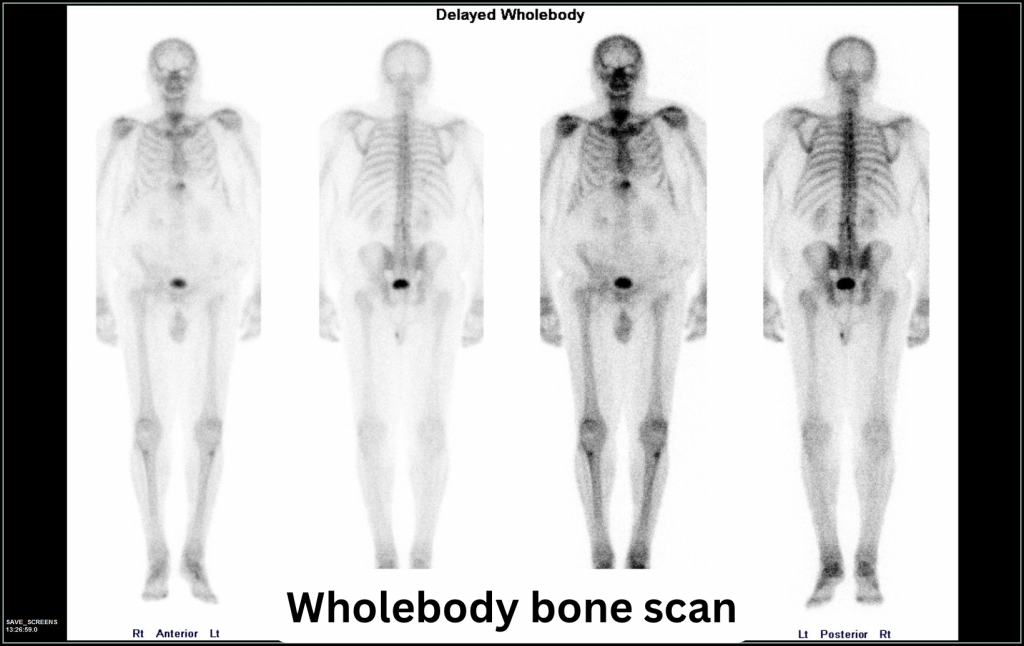
Bone scan injection for lower back pain with immediate images performed.
8:15am
Bone scan injection for metastatic prostate cancer.
8:30am
Thyroid scan for a multinodular goiter with imaging performed 20 minutes after injection. The radiopharmaceutical demonstrates any areas of the thyroid that may have nodules that are producing too many hormones.
9am
Cardiac resting and stress scan for chest pain. Resting images are performed 20 minutes after injection.
The patient then undergoes pharmacological stress test where a medication is administered to mimic the effects of exercise on the heart before another injection of the radiopharmaceutical.
10am
Bone scan injection is performed for someone with a stress fracture unable to be visualised on CT and x-ray. Initial images are performed.
10:30am
Cardiac stress imaging performed. Hybrid and cardiac rhythm imaging is performed of both the rest and stress images for anatomical correlation and to visualise the pumping of the heart.
11am
The first bone scan returns for their delayed imaging. A whole body image is performed as well as hybrid 3D images of their lower back.
12pm
The second bone scan returns. A whole body image is performed as well as a 3D hybrid image of the area of interest.
1pm
The final bone scan returns. Localised imaging is performed of the ankle as well as a 3D hybrid image of the ankle.
2pm
Liver imaging is performed on a patient who is experiencing pain after eating to identify if the patient has a blockage in the gallbladder. After injection dynamic (flow) imaging is performed to visualise the movement of the radiopharmaceutical through the liver and the gallbladder.
A fatty meal is ingested by the patient while the imaging is being performed to initiate the contraction of the bladder. This scan generally takes 2 hours, with the meal given at the 1 hour point.
4pm
Turn everything off, make sure all the images are sent to the reporting doctors, and go home!

It is important to note that as a technologist we must consult every patient to get their clinical history, ensure the correct scans are being performed as well as ensuring that all correct preparation has been done for the scan.
Once that scan has been performed you process the images prior to being sent to the reporting doctor. Processing images can involve performing calculations as well as ensuring that they are clear and accurate.
This is just what one day will look like and no two days are the same!
There are so many different scans that can be performed and all for different reasons.
Nuclear medicine has multiple different aspects in which technologists are a part of and the types of scans that can be performed are just as diverse as the patients!
There are endless career opportunities as well as opportunity for career advancement. Nuclear medicine is always evolving and growing which will provide a career that will always have ongoing learning.